Provided by:

Are these patients really enjoying life more? Granted, having a beautiful smile does make someone smile more, being able to eat better does improve their quality of life and not having any oral infections will help keep the body healthier. Dentists today are able to have significant impact on the whole body health and make a real impact on patients accurately feeling better and improving some or many of the chronic medical conditions facing patients today.
The time is now here for DSO dentists to take on the responsibility of recognizing patients at risk of sleep disorders. The dental team is in a unique position to have the opportunity to screen and treat sleep disorders. Treating patients with a sleeping disorder can also opening the potential for increased increased revenues and add quality of life to those patients and likely save lives as well.
Why would DSO dentists want to start providing dental sleep medicine? The American Dental Association’s states : “The adopted policy statement outlines the role of dentists in treating SRBD. Key components include assessing a patient’s risk for SRBD as part of a comprehensive medical and dental history and referring affected patients to appropriate physicians (ADA website). As with oral cancer screenings the ADA states: All adult dental patients should receive an intraoral and extraoral conventional visual and tactile examination when visiting their dentists. The Oral Cancer Foundation estimates that just shy of 50,000 people are diagnosed with oral oropharyngeal cancer annually, and oral cancer will lead to more than 9,750 deaths a year. The American Academy of Dental Sleep Medicine pegs the number of adults in the U.S. who have obstructive sleep apnea at 30 million or more that’s one out of every ten citizens who are at least 18 years of age.
Deaths attributed to a sleep breathing disorder is hard to estimate due to the many comorbidities that it causes, automobiles accidents brought upon by falling asleep while driving, or sleepy driving or the innocent bystander caught in the way.
The dental team is usually the medical team that sees the patient more than other practitioners when the patient is feeling healthy. The fact is that all dentists have an obligation to screen for sleep related disorders according to the American Dental Association.
Approximately 50-70 million people in the United States are chronic sufferers from sleep disorder, who have impaired health and daily functioning issues as a result of those disorders (Attanasio, 2010). The DSO dental team can ascertain the structures of the craniofacial that can contribute to the possibility of a sleep breathing disorder such as size or oropharyngeal, soft palate, tongue, arch size and hard palate to name a few. The team is available to ask many of the questions that signal that a patient is not feeling as well as their peers. If a structured screening questionnaire is not used then most of what is done during a routine dental visit can be applied as a screening. Updating a patient’s health history identify comorbidities such as heart disease, diabetes, depression, or anxiety, and age which can be indicators of an underlying undiagnosed sleep condition. The direct observation of the patients by noticing if they are obese, have a large neck, or if the patient is a mouth breather. Causal conversation with patients can find out is a patient sleeps well, is tired all the time, or a gets up often during the night to use the bathroom.
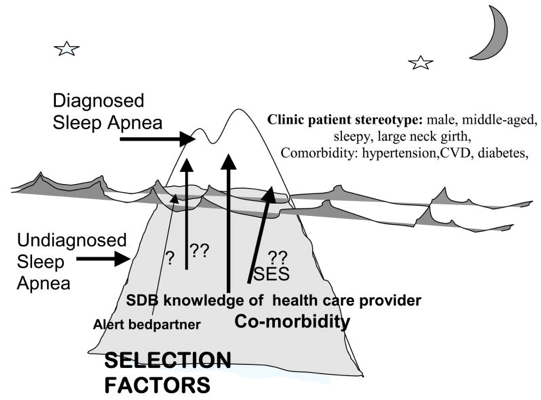
Selection biases for clinical recognition and diagnosis of sleep apnea. The proportion of all cases of sleep apnea is represented by the iceberg, with clinically diagnosed cases shown in the tip of the iceberg. Clinically recognized sleep apnea represents less than 85% of the total prevalence of sleep apnea cases that would be candidates for treatment. Factors that favor selection of individuals with unrecognized sleep apnea (below the tip of the iceberg) for clinical referral and diagnosis are shown (Young, 2009).
Once these patients are identifies the DSO dental team (dentist or hygienist) should have a conversation with the patient, just like if a suspicious area were found for referring to an oral surgeon for a more thorough evaluation, the patient should be referred to their physician with a follow-up on what was observed.
On the other hand, why wouldn’t a DSO dentist not want to practice treating their patients with oral appliance therapy?”Adding OSA (Obstructive Sleep Apnea) treatment can be profitable for the DSO dental practice. Oral appliance therapy is a $220 million annual market and growing.
“The market for dental sleep medicine is rising primarily because of unmet medical needs.
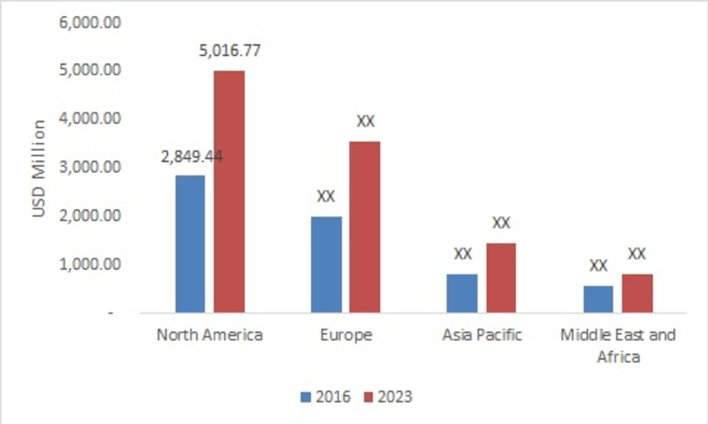
North America was the largest market for global dental sleep medicine in 2016. The North American market is led by the U.S. due to high per capita income, better reimbursement policy for medical devices, and larger healthcare market. Also, the concentration of major medical device manufacturers in the U.S. drives the growth of the North American market.” (Market research futures, 2017)
Dental sleep medicine is a separate specialty from traditional dentistry. If you’re one of the first to consider practicing dental sleep medicine, you’re are an early adopter in the field. This gives the DSO the opportunity to master the practice with little or no competition.
Each DSO dental practice, without attracting patients from outside their practice has the potential to generate hundreds of cases annually. Approximately, 1 in 4 patients in the average practice has a sleep breathing disorder.
Nothing in dentistry thus far has created new relationships with our brethrens in the medical community. Providing dental sleep medicine gives dental providers the chance to sharpen their skills in medicine and gain new information to better serve patients in a way unimaginable before. Creating relationships with the surrounding medical associations helps strengthen the bond to form a strategic exchange for referring patients, finally providing co-patient care. For coverage under medical insurance, by law, a board-certified physician must make the diagnosis and write a RX for the oral appliance. This empowerment of interdisciplinary care models help creating an exchange to have the physicians refer non-compliant CPAP users to the office as well. In return, the dental team refers patients for sleep evaluations and/or sleep testing to the physician, with the ultimate goal of treating the total patient health.
The revenues generated for providing dental sleep medicine can be generated by the newly trained sleep team, meaning most of the appointments can be completed by the staff, from the start of patients walking into the waiting room, to final insertion of the appliance and follow-up adjustment appointments. The dentist involvement is minimal with the confirming the outcome of the screening by the hygienist, reading the sleep test to the patient, possible taking the impressions (although a hygienist can be trained to perform this), confirming fit of the oral appliance and finally making any adjustments.. No real production time needs to be used for treating dental sleep medicine. This revenue generating should be done by the well-trained dental team members. And, patients who sleep better, feel better and are an excellent source of referrals from family, friends and those they work with!